The actor Gene wilder died yesterday, from complications of Alzheimer's Disease,
He was in some of my very favorite funny movies, including The Producers and Young Frankenstein, both of which, I am happy to say, my children also love. I want to link to a favorite scene, but I'm having trouble finding just one. I think this one is as good as any:
I just love his manic, panicked voice, which came out in a lot of his work. And that scene was followed up immediately by this one, which is just as great.
But more than just making me laugh a lot, Gene Wilder has another place in my heart: he was the first celebrity that I featured in this blog who had lymphoma. I wrote about it just about a month after I was diagnosed. Wilder had Mantle Cell Lymphoma, went through chemo, and then had a stem cell transplant, which put him in remission.
It wasn't Follicular Lymphoma, but I didn't care. I was happy to know that someone came out alright. Even better if it was someone who made me laugh.
A lot had been made, in these last 24 hours, of Wilder's work with cancer, not just because he was a survivor, but because his wife Gilda Radner was not. She died from ovarian cancer, and Wilder helped found Gilda's Club, where cancer patients can go for support. (I wrote about that a few years ago, too.)
He was a big advocate of early detection; Radner's cancer was misdiagnosed for a long time (too common in ovarian cancer), and her cancer was far advanced by the time she did get the right diagnosis. So Wilder's legacy, at least for some people, will be about his support for cancer patients, as much as his very funny movies.
But the thing that both Gene Wilder and Gilda Radner reminded me of was to see the humor in my situation. I guess I have that outlook naturally, anyway -- I can see the absurd humor in just about anything. But the reminder is always nice. Gilda, a very funny woman (funnier than her husband, really -- he was a better comic actor, but she just damn funny), once said, "Cancer is probably the most unfunny thing in the world, but I'm a comedian, and even cancer couldn't stop me from seeing the humor in what I went through."
Words to live by.
So I'm sad to hear about Gene Wilder, but I will certainly remember the joy he brought me -- and the great things he did for us.
Tuesday, August 30, 2016
Thursday, August 25, 2016
PET Predicts Survival?
Very interesting research published a few days ago in the Journal of Clinical Oncology called "Baseline Metabolic Tumor Volume Predicts Outcome in High-Tumor-Burden Follicular Lymphoma: A Pooled Analysis of Three Multicenter Studies."It has some significant implications for diagnosing aggressive forms of Follicular Lymphoma.
There have been a couple of FL issues from the last couple of months that kind of come together in this article. First, there's the issue of PET scans, which have been shown to be very useful as a baseline measure at diagnosis, and again after a treatment has been completed. Gives the doctor something to compare to.
Then there's the issue of trying to identify more aggressive Follicular Lymphoma as early as possible, so treatment can be matched up with it and the disease fought aggressively. There has been some recent research that focused on the m7-FLIPI model and POD24 -- trying to figure out of a patient is in that group that will have Progression of Disease within 24 months. There's a feeling that being able to identify an aggressive FL early will perhaps allow it to treated more effectively.
The research from the JCO is related to those things. It shows some value in using a PET scan to figure out if a patient has a more aggressive type of FL.
Now, the PETs that I get come back with a number that measures the widest point of my swollen nodes. It will say something like "One inguinal node 5 cm; two chestal nodes, 6 cm and 3 cm" (I forget what nodes in the chest are called, so I'm going with "chestal." Thoracic, maybe? I'll look it up later.) That way of measuring certainly tells you something, and if you're comparing from scan to scan, it works fine by showing that nodes are growing or shrinking.
But the researchers in this study measured nodes in a different way -- by volume. So the measure not just the widest point of the nodes, but also how long the are and how deep they are. (I had to ask my kids how to measure volume. I haven't done that since high school. Height X width X depth.) Think about it as not how much liquid all of those nodes could hold if you filled them up.
What they found was that, if you added up the volume of all of those nodes, then a total of 510 cubic centimeters was a significant number. Higher than that at diagnosis, and the Progression Free Survival (the time it took for the disease to get worse) was less than 3 years. Less than 510, and the the PFS was over 6 years. The higher volume also predicted that progression was likely to happen within 1 to 2 years (back to that POD24 again).
(In case you are wondering how much 510 cubic centimeters is, it's a little more than half a liter, or a little more than 17 fluid ounces. So you could fit all of your swollen nodes into a Grande at Starbucks, or a decent sized bottle of Coke.)
The researchers went further and compared results to FLIPI2 scores. (See Lymphomation for a discussion of FLIP and FLIPI2.) Together, the FLIPI2 and the node volume seem to be able to predict pretty well which patients will need treatment within 24 months.
By looking at the node volume and the FLIPI2 score, they were able to create three groups of patients, based on they were to reach a 5 year Progression Free Survival. Patients with low volume (below 510 cubic centimters) and a low FLIPI2 score had a 69% chance. A high volume OR a high FLIPI2 had a 46% chance. And a high volume AND a high FLIPI2 had just a 20% chance.
It's an interesting idea. It's important to remember, however, that this is not a perfect predictor. But it might give doctors a potential tool for figuring out which patients are at greatest risk for progressing early, and maybe giving them a better chance at getting more aggressive treatment early.
Some things to think about?
That volume measurement is actually called Total Metabolic Tumor Volume, and doesn't actually involve measuring the height, width, and depth -- the volume is determined with a statistical formula that estimates how much volume is there. It estimates it very well, but it's still not a perfect measure, so that 510 might not be exact. And, of course, everyone is different. No one mathces up perfectly with the statistics.
On top of all of that, the standard measurement for nodes in a PET is still to measure that widest point. I'm not sure how much work needs to be done by someone reading a PET scan to go from a one dimensional measurement to a three dimensional measurement.
So, this information isn't going to affect your next scan, most likely.
But it could end up being very useful in the future. I like that there is so much work being done to identify patients who are at risk of early progression. Even though I'm now in that group, the more we know about a sub-group, the more we'll likely know about the rest of us, too.
There have been a couple of FL issues from the last couple of months that kind of come together in this article. First, there's the issue of PET scans, which have been shown to be very useful as a baseline measure at diagnosis, and again after a treatment has been completed. Gives the doctor something to compare to.
Then there's the issue of trying to identify more aggressive Follicular Lymphoma as early as possible, so treatment can be matched up with it and the disease fought aggressively. There has been some recent research that focused on the m7-FLIPI model and POD24 -- trying to figure out of a patient is in that group that will have Progression of Disease within 24 months. There's a feeling that being able to identify an aggressive FL early will perhaps allow it to treated more effectively.
The research from the JCO is related to those things. It shows some value in using a PET scan to figure out if a patient has a more aggressive type of FL.
Now, the PETs that I get come back with a number that measures the widest point of my swollen nodes. It will say something like "One inguinal node 5 cm; two chestal nodes, 6 cm and 3 cm" (I forget what nodes in the chest are called, so I'm going with "chestal." Thoracic, maybe? I'll look it up later.) That way of measuring certainly tells you something, and if you're comparing from scan to scan, it works fine by showing that nodes are growing or shrinking.
But the researchers in this study measured nodes in a different way -- by volume. So the measure not just the widest point of the nodes, but also how long the are and how deep they are. (I had to ask my kids how to measure volume. I haven't done that since high school. Height X width X depth.) Think about it as not how much liquid all of those nodes could hold if you filled them up.
What they found was that, if you added up the volume of all of those nodes, then a total of 510 cubic centimeters was a significant number. Higher than that at diagnosis, and the Progression Free Survival (the time it took for the disease to get worse) was less than 3 years. Less than 510, and the the PFS was over 6 years. The higher volume also predicted that progression was likely to happen within 1 to 2 years (back to that POD24 again).
(In case you are wondering how much 510 cubic centimeters is, it's a little more than half a liter, or a little more than 17 fluid ounces. So you could fit all of your swollen nodes into a Grande at Starbucks, or a decent sized bottle of Coke.)
The researchers went further and compared results to FLIPI2 scores. (See Lymphomation for a discussion of FLIP and FLIPI2.) Together, the FLIPI2 and the node volume seem to be able to predict pretty well which patients will need treatment within 24 months.
By looking at the node volume and the FLIPI2 score, they were able to create three groups of patients, based on they were to reach a 5 year Progression Free Survival. Patients with low volume (below 510 cubic centimters) and a low FLIPI2 score had a 69% chance. A high volume OR a high FLIPI2 had a 46% chance. And a high volume AND a high FLIPI2 had just a 20% chance.
It's an interesting idea. It's important to remember, however, that this is not a perfect predictor. But it might give doctors a potential tool for figuring out which patients are at greatest risk for progressing early, and maybe giving them a better chance at getting more aggressive treatment early.
Some things to think about?
That volume measurement is actually called Total Metabolic Tumor Volume, and doesn't actually involve measuring the height, width, and depth -- the volume is determined with a statistical formula that estimates how much volume is there. It estimates it very well, but it's still not a perfect measure, so that 510 might not be exact. And, of course, everyone is different. No one mathces up perfectly with the statistics.
On top of all of that, the standard measurement for nodes in a PET is still to measure that widest point. I'm not sure how much work needs to be done by someone reading a PET scan to go from a one dimensional measurement to a three dimensional measurement.
So, this information isn't going to affect your next scan, most likely.
But it could end up being very useful in the future. I like that there is so much work being done to identify patients who are at risk of early progression. Even though I'm now in that group, the more we know about a sub-group, the more we'll likely know about the rest of us, too.
Saturday, August 20, 2016
Duvelisib Trial
OncLive has been producing some interesting videos lately, mostly of experts in oncology discussing recent developments in the field.
The most recent is a series of videos focusing on PI3 kinase inhibitors, featuring Dr. Ian Flinn and Dr. Jennifer Brown. You can watch all four videos in the series at the same link, though I'm mostly going to focus on Dr. Finn's discussion of Duvelisib.
First, some background (some of this is covered in the other videos in the series, and you can always read about lots of targeted pathway treatments at Lymphomation.org).
Duvelisib is a type of Kinase Inhibitor. The other Kinase Inhibitors that get talked about a lot in Follicular Lymphpoma circles are Idelalisib and Ibrutinib. Duvelisib and Idelalisib are examples of PI3 Kinase Inhibitors, so it makes sense to look at them together (which the OncLive videos do).
In general, a protein kinase is a kind of enyzme that attaches to other proteins to allow them to help a cell function, by growing or dividing or doing its basic job. So a Kinase Inhibitor is a treatment that inhibits a Kinase from attaching to the those proteins. If you look at the Lymphomation link above, you'll see that inhibitors are part of a larger group of treatments called pathway targeting treatments -- a kinase allows the cell to perform an action, and when that action is done, it allows another action to happen, etc., etc., almost like a pathway. So if you cut off one of those actions, the rest of the pathway can't happen. Inhibit a kinase from attaching to a protein, and it messes up the rest of the cell's pathway. Do that to a cancer cell, and you keep the cancer from growing.
PI3 (short for Phosphoinositide 3) Kinase inhibitors focus on a specific part of a larger pathway known as the PI3K/AKT/mTOR pathway. Just like other pathway targeting treatments, messing with one part of this pathway will shut the whole thing down, and there are treatments that target AKT and mTOR in different stages of development. This pathway is important for a cancer cell being able to grow, feed itself, and copy itself, so messing it up will mean that the cell can't grow and divide and do the bad things that makes cancer so horrible.
But of course, nothing is easy when it comes to cancer.
In the body, proteins have different isoforms. This means when they get copied, they don't come out exactly the same. They might be pretty close to the same, but they aren't exact. This is actually a good thing, usually. It allows for protein diversity, and in evolution, diversity is a good thing.
Imagine it this way -- you make a batch of chocolate chip cookies. The first dozen come out a little crispy, so with the second batch, you take them out a minute sooner, so they are less crispy and more chewy. The third batch, you forgot about, so they stay in three minutes longer and are downright hard. Same recipe, three very different cookies. Fortunately, you have three kinds who drive you crazy by not agreeing on anything, and one likes chewy cookies, one likes crispy cookies, and one likes them hard so she can dunk them in milk. Same recipe, three different cookies, but three happy outcomes. No one complains about the cookies. Diversity is good.
Same with protein isoforms. One protein that gets copied, but with slight variations. They all came from the same source (or recipe) and they all do the same function (make your kids shut up because they aren't really hungry, just bored, because it's summer and they won't admit that they really do want to go back to school).
So, to get back to PI3 Kinase inhibitors. Naturally, they have different isoforms, known as p110 alpha, p110 beta, p110 gamma, and p110 delta. Without knowing that, someone could think they are targeting all PI3 kinase, but are really only targeting one isoform.
Fortunately, researchers are aware of the different isoforms. Idelalisib targets the p110 delta isoform, and Duvelisib both gamma and delta isoforms.
There are a bunch of other PI3 kinase inhibitors in different stages of testing, targeting differennt isoforms and different cancers, including a few more for Follicular Lymphoma.
Dr. Finn's video on Duvelisib discusses a particular phase I clinical trial that looked at single agent Duvelisib (it has been in other trials as a combination treatment with other agents). This trial looked at Duvelisib as a treatment for patients who had tried Rituxan and chemo and were no longer seeing any results from them. Early results for single-agent Duvelisib look great -- 70% Overall Response with "nearly one third" having a Complete Response.
The four videos focus in PI3 Kinase inhibitors, but they touch on lots of different treatments (Dr. Finn is excited about R squared). Worth watching.
Hope the background info helped.
Always nice to know we have some more potential arrows for our quivers.
The most recent is a series of videos focusing on PI3 kinase inhibitors, featuring Dr. Ian Flinn and Dr. Jennifer Brown. You can watch all four videos in the series at the same link, though I'm mostly going to focus on Dr. Finn's discussion of Duvelisib.
First, some background (some of this is covered in the other videos in the series, and you can always read about lots of targeted pathway treatments at Lymphomation.org).
Duvelisib is a type of Kinase Inhibitor. The other Kinase Inhibitors that get talked about a lot in Follicular Lymphpoma circles are Idelalisib and Ibrutinib. Duvelisib and Idelalisib are examples of PI3 Kinase Inhibitors, so it makes sense to look at them together (which the OncLive videos do).
In general, a protein kinase is a kind of enyzme that attaches to other proteins to allow them to help a cell function, by growing or dividing or doing its basic job. So a Kinase Inhibitor is a treatment that inhibits a Kinase from attaching to the those proteins. If you look at the Lymphomation link above, you'll see that inhibitors are part of a larger group of treatments called pathway targeting treatments -- a kinase allows the cell to perform an action, and when that action is done, it allows another action to happen, etc., etc., almost like a pathway. So if you cut off one of those actions, the rest of the pathway can't happen. Inhibit a kinase from attaching to a protein, and it messes up the rest of the cell's pathway. Do that to a cancer cell, and you keep the cancer from growing.
PI3 (short for Phosphoinositide 3) Kinase inhibitors focus on a specific part of a larger pathway known as the PI3K/AKT/mTOR pathway. Just like other pathway targeting treatments, messing with one part of this pathway will shut the whole thing down, and there are treatments that target AKT and mTOR in different stages of development. This pathway is important for a cancer cell being able to grow, feed itself, and copy itself, so messing it up will mean that the cell can't grow and divide and do the bad things that makes cancer so horrible.
But of course, nothing is easy when it comes to cancer.
In the body, proteins have different isoforms. This means when they get copied, they don't come out exactly the same. They might be pretty close to the same, but they aren't exact. This is actually a good thing, usually. It allows for protein diversity, and in evolution, diversity is a good thing.
Imagine it this way -- you make a batch of chocolate chip cookies. The first dozen come out a little crispy, so with the second batch, you take them out a minute sooner, so they are less crispy and more chewy. The third batch, you forgot about, so they stay in three minutes longer and are downright hard. Same recipe, three very different cookies. Fortunately, you have three kinds who drive you crazy by not agreeing on anything, and one likes chewy cookies, one likes crispy cookies, and one likes them hard so she can dunk them in milk. Same recipe, three different cookies, but three happy outcomes. No one complains about the cookies. Diversity is good.
Same with protein isoforms. One protein that gets copied, but with slight variations. They all came from the same source (or recipe) and they all do the same function (make your kids shut up because they aren't really hungry, just bored, because it's summer and they won't admit that they really do want to go back to school).
So, to get back to PI3 Kinase inhibitors. Naturally, they have different isoforms, known as p110 alpha, p110 beta, p110 gamma, and p110 delta. Without knowing that, someone could think they are targeting all PI3 kinase, but are really only targeting one isoform.
Fortunately, researchers are aware of the different isoforms. Idelalisib targets the p110 delta isoform, and Duvelisib both gamma and delta isoforms.
There are a bunch of other PI3 kinase inhibitors in different stages of testing, targeting differennt isoforms and different cancers, including a few more for Follicular Lymphoma.
Dr. Finn's video on Duvelisib discusses a particular phase I clinical trial that looked at single agent Duvelisib (it has been in other trials as a combination treatment with other agents). This trial looked at Duvelisib as a treatment for patients who had tried Rituxan and chemo and were no longer seeing any results from them. Early results for single-agent Duvelisib look great -- 70% Overall Response with "nearly one third" having a Complete Response.
The four videos focus in PI3 Kinase inhibitors, but they touch on lots of different treatments (Dr. Finn is excited about R squared). Worth watching.
Hope the background info helped.
Always nice to know we have some more potential arrows for our quivers.
Tuesday, August 16, 2016
Oncologist Appointment
I had an oncologist appointment today.
The good news: Everything looks great.
The not-so-good news: I think I'm going to look for a new oncologist.
First, my health. Everything looks great. My blood work was "100% perfect," according to Dr. K. His physical exam didn't show any problems, either. And I feel fine. So, in my usual three-part exam, I was 3 for 3. All good.
Now, as for my wanting a new oncologist......
I've been seeing Dr. K for a little over a year now, and if you've read that far back, you know I haven't been all that crazy about him from the start. I am aware that he had a tough act to follow. Dr. R was my first oncologist, and I think we get attached to our doctors when they have guided us through rough times (like a cancer diagnosis and treatment). But Dr. R was also (1) young, which I think made him more sensitive to patient needs, (2) a hematology specialist, which made it easier to have conversations about Follicular Lymphoma and its treatments, and (3) just a nice guy -- we'd spend the first 10 minutes of the appointment talking about my kids, his kids, baseball, whatever. He put me at ease, and oncology appointments were almost (almost) something to look forward to.
Dr. K really isn't any of those things. He's close to retirement, which isn't a bad thing in and of itself, though it had Dr. R a little worried about recommending him, thinking he may retire soon and I'd need to switch doctors sooner than I'd hoped to (which is kind of ironic). The website for the practice lists hematology as one of his specialties, but his approach seems to be to look up NCCN Guidelines for how to treat Follicular Lymphoma, and then just do what they say. Again, not necessarily a bad thing, but if the reason for everything you do it "because the book says so," it doesn't leave any room for discussion. And he does seem to be a nice guy, but I always feel like he has no idea who I am, and doesn't care to know. It's not that he is unkind or inhumane, but it's like he didn't even bother to look at (or take) any notes before he comes into the room. But when your plan is to follow what the book says, those little differences between patients don't really matter, right?
So for today's appointment, he came into the room, rubbing antibacterial foam into his hands (he doesn't shake hands or anything like that), and told me that my blood work was "100% perfect." He then went down the list of everything that gets looked at in a Complete Blood Panel, using the most general terms he could, like "clotting cells" instead of "platelets." And then he said, "So everything looks great, but I'm going to throw in a twist." I waited. "I want you to get a CT scan," he said.
I told him that I thought I had gotten one a year ago. Turns out it was 2 years ago, in June 2014. Fine. "Do I need a CT scan?" I asked.
"Well, I think it would be a good idea to take a look inside. Just to get another baseline. I don't think we'll find anything, maybe a few slightly swollen nodes. But I think it would be a good idea to see what's going on."
He then asked me to take off my shirt and he did the physical exam, feeling my nodes and checking my eyes and lungs and throat, all the while repeating three or four more times that he thought a CT scan would be a good idea.
He was aware that unnecessary radiation could be a problem. But he still thought a CT was a good idea.
At this point, he asked me how my summer was going. I started to tell a story about my son. He interrupted and told me his own story about being in medical school. Then he said, "OK. Everything looks great. I'll let you get out of here and do what you need to do today." And he was gone.
I made my way to the exit, stopping at the desk to make another appointment for 6 months. I think I was supposed to make a scan appointment then, but I didn't. By the time I got to my car, I had decided that it was time to look for a new oncologist.
At this point in my life as a cancer patient, I know what I want and need from a doctor. And I'm not going to bother with one if I'm not getting what I need.
I need someone who treats me like an individual. I don't expect someone to remember the details of my life 6 months after I tell them to him. But I do expect him to listen when I am telling them. I remember my first appointment with him. He seemed to have a prepared speech for patients with Follicular Lymphoma, giving some very basic information.Which might have been fine if I had just been diagnosed. But I already had 7 years as a patient. And when I tried to explain that I do a lot of research, he was dismissive. I called myself a "cancer nerd," and he said, "No no not, you're not a nerd," and then kind of gave me a little pep talk about self-esteem, completely ignoring what I had to say about the level of conversation I was willing to engage in.
It's been the same pattern in all of my visits -- he has a prepared speech, he doesn't seem interested in any kind of discussion, he interrupts and doesn't listen, and there's really no room for anything other that what the Guidelines say.
And I thought all of that would be fine. I thought as long as I'm healthy, all I really need is someone to order order blood work and feel my nodes every 4 to 6 months. If and when I need treatment, I can go to a specialist for a second opinion, and have him or her deal with the heavy stuff.
But I just can't do it any more.
I've already started looking. In some ways, another general oncologist would be good, someone who knows how to talk to patients and treat them like people. In other ways, a lymphoma specialist would be good, someone who can say "There's been some interesting research on a new Immunotherapy treatment" when I ask what's new.
I'd be happy with either. I used to have both. Now I have neither.
I don't know who I will see for my next oncology appointment, but I'm pretty sure it won't be Dr. K. And I'm pretty sure I won't be getting an unnecessary CT scan, either.
I'm not happy about it all.
I'll keep you updated.
The good news: Everything looks great.
The not-so-good news: I think I'm going to look for a new oncologist.
First, my health. Everything looks great. My blood work was "100% perfect," according to Dr. K. His physical exam didn't show any problems, either. And I feel fine. So, in my usual three-part exam, I was 3 for 3. All good.
Now, as for my wanting a new oncologist......
I've been seeing Dr. K for a little over a year now, and if you've read that far back, you know I haven't been all that crazy about him from the start. I am aware that he had a tough act to follow. Dr. R was my first oncologist, and I think we get attached to our doctors when they have guided us through rough times (like a cancer diagnosis and treatment). But Dr. R was also (1) young, which I think made him more sensitive to patient needs, (2) a hematology specialist, which made it easier to have conversations about Follicular Lymphoma and its treatments, and (3) just a nice guy -- we'd spend the first 10 minutes of the appointment talking about my kids, his kids, baseball, whatever. He put me at ease, and oncology appointments were almost (almost) something to look forward to.
Dr. K really isn't any of those things. He's close to retirement, which isn't a bad thing in and of itself, though it had Dr. R a little worried about recommending him, thinking he may retire soon and I'd need to switch doctors sooner than I'd hoped to (which is kind of ironic). The website for the practice lists hematology as one of his specialties, but his approach seems to be to look up NCCN Guidelines for how to treat Follicular Lymphoma, and then just do what they say. Again, not necessarily a bad thing, but if the reason for everything you do it "because the book says so," it doesn't leave any room for discussion. And he does seem to be a nice guy, but I always feel like he has no idea who I am, and doesn't care to know. It's not that he is unkind or inhumane, but it's like he didn't even bother to look at (or take) any notes before he comes into the room. But when your plan is to follow what the book says, those little differences between patients don't really matter, right?
So for today's appointment, he came into the room, rubbing antibacterial foam into his hands (he doesn't shake hands or anything like that), and told me that my blood work was "100% perfect." He then went down the list of everything that gets looked at in a Complete Blood Panel, using the most general terms he could, like "clotting cells" instead of "platelets." And then he said, "So everything looks great, but I'm going to throw in a twist." I waited. "I want you to get a CT scan," he said.
I told him that I thought I had gotten one a year ago. Turns out it was 2 years ago, in June 2014. Fine. "Do I need a CT scan?" I asked.
"Well, I think it would be a good idea to take a look inside. Just to get another baseline. I don't think we'll find anything, maybe a few slightly swollen nodes. But I think it would be a good idea to see what's going on."
He then asked me to take off my shirt and he did the physical exam, feeling my nodes and checking my eyes and lungs and throat, all the while repeating three or four more times that he thought a CT scan would be a good idea.
He was aware that unnecessary radiation could be a problem. But he still thought a CT was a good idea.
At this point, he asked me how my summer was going. I started to tell a story about my son. He interrupted and told me his own story about being in medical school. Then he said, "OK. Everything looks great. I'll let you get out of here and do what you need to do today." And he was gone.
I made my way to the exit, stopping at the desk to make another appointment for 6 months. I think I was supposed to make a scan appointment then, but I didn't. By the time I got to my car, I had decided that it was time to look for a new oncologist.
At this point in my life as a cancer patient, I know what I want and need from a doctor. And I'm not going to bother with one if I'm not getting what I need.
I need someone who treats me like an individual. I don't expect someone to remember the details of my life 6 months after I tell them to him. But I do expect him to listen when I am telling them. I remember my first appointment with him. He seemed to have a prepared speech for patients with Follicular Lymphoma, giving some very basic information.Which might have been fine if I had just been diagnosed. But I already had 7 years as a patient. And when I tried to explain that I do a lot of research, he was dismissive. I called myself a "cancer nerd," and he said, "No no not, you're not a nerd," and then kind of gave me a little pep talk about self-esteem, completely ignoring what I had to say about the level of conversation I was willing to engage in.
It's been the same pattern in all of my visits -- he has a prepared speech, he doesn't seem interested in any kind of discussion, he interrupts and doesn't listen, and there's really no room for anything other that what the Guidelines say.
And I thought all of that would be fine. I thought as long as I'm healthy, all I really need is someone to order order blood work and feel my nodes every 4 to 6 months. If and when I need treatment, I can go to a specialist for a second opinion, and have him or her deal with the heavy stuff.
But I just can't do it any more.
I've already started looking. In some ways, another general oncologist would be good, someone who knows how to talk to patients and treat them like people. In other ways, a lymphoma specialist would be good, someone who can say "There's been some interesting research on a new Immunotherapy treatment" when I ask what's new.
I'd be happy with either. I used to have both. Now I have neither.
I don't know who I will see for my next oncology appointment, but I'm pretty sure it won't be Dr. K. And I'm pretty sure I won't be getting an unnecessary CT scan, either.
I'm not happy about it all.
I'll keep you updated.
Friday, August 12, 2016
Pan Pacific Lymphoma Conference: Videos
A couple of weeks ago, I wrote about a video from the Pan Pacific Lymphoma Conference on staging FL with PET scans. It turns out there are a few more videos available from that conference (all from ASCO Post). I thought about stretching them out into several posts, but it's probably easier to give links to all of them in a single post.
So here are the videos from that conference that I found most interesting:
John G. Gribben, MD, DSc, on Follicular Lymphoma: Still a Role for Transplant?
Dr. Gribben discusses Autologous Stem Cell Transplants (where the stem cells come from the patient herself) and Allogeneic Stem Cell Transplants (where the cells come from a donor), and the potential problems for each. As he points out, Follicular Lymphoma is especially challenging, because it is considered incurable, and because there is no course of treatment that oncologists agree on. And as new treatments are being developed, the question is whether or not transplants are worth considering. He thinks there is, especially for young patients with aggressive disease, who can handle aggressive chemo, and start with an Auto SCC and move to an Allo SCT if necessary. A nice summary of what goes into that decision.
Fredrick B. Hagemeister, Jr, MD, on Using Rituximab Maintenance
Dr. Hagemeister addresses the issues surrounding Rituxan Maintenance. And there are many, as I have been saying for a few years, as one study seems to say that RM is a great thing, and then another seems to say it's not worth it (and then this pattern is repeated). The issue, says Dr. Hagemeister, is Progression-Free Survival, and since most patients would say they would like to go as long as possible between treatments, Rituxan Maintenance should be considered. He was at the conference to speak in favor of RM, and thinks there is still a role for maintenance for certain patients. (Dr. Hagemeister gets extra points for saying that patients should have a voice in choosing treatments, as long as they have all of the information to make a good decision. And while he doesn't necessarily label it this way, I think he sees the importance of the emotional factor that goes into making this decision. Follicular Lymphoma is an emotional disease as well as a physical one -- I like to hear a doctor who recognizes that.)
Nathan Fowler, MD, and Sagar Lonial, MD, on Treating Follicular Lymphoma
This video has a pretty general title, but there really is more of a focus to it -- Dr. Fowler and Dr. Lonial discuss how to treat Follicular Lymphoma which is refractory or relapsed "early" (which they define as within 2 years after treatment). Dr. Fowler presented at the conference on the recent studies that showed that patients who relapsed within 2 years after receiving R-CHOP had shorter median Overall Survivals. He refers to Dr. Bruce Cheson's talk about PET scans -- a PET at diagnosis can offer a baseline to compare to, if a PET is then taken after treatment. PET scans after treatment can help determine if a patient is likely to be in that POD24 group. Dr. Fowler lists some of the choices that patients have if they are in that "early" group, including Bendamustine, Idilisib, and Obinituzimab. Still, the choice is tough. Dr. Fowler's own personal approach is to try Bendamustine if R-CHOP fails, and if Bendamustine fails within 18 months, he would seriously consider a transplant.
So, some interesting videos, mostly summarizing some of the recent advancements in the field.
Also, I love the ukulele music. I was so distracted by Dr. Cheson's cool shirt in the last video from two weeks ago that I didn't even notice the music.
My dream is to have a job that has conferences in Hawaii. Until that happens, I couldn't think of a group of people (oncologists and cancer researchers) that deserves it more.
Treating FL
https://vimeo.com/174702741
So here are the videos from that conference that I found most interesting:
John G. Gribben, MD, DSc, on Follicular Lymphoma: Still a Role for Transplant?
Dr. Gribben discusses Autologous Stem Cell Transplants (where the stem cells come from the patient herself) and Allogeneic Stem Cell Transplants (where the cells come from a donor), and the potential problems for each. As he points out, Follicular Lymphoma is especially challenging, because it is considered incurable, and because there is no course of treatment that oncologists agree on. And as new treatments are being developed, the question is whether or not transplants are worth considering. He thinks there is, especially for young patients with aggressive disease, who can handle aggressive chemo, and start with an Auto SCC and move to an Allo SCT if necessary. A nice summary of what goes into that decision.
Fredrick B. Hagemeister, Jr, MD, on Using Rituximab Maintenance
Dr. Hagemeister addresses the issues surrounding Rituxan Maintenance. And there are many, as I have been saying for a few years, as one study seems to say that RM is a great thing, and then another seems to say it's not worth it (and then this pattern is repeated). The issue, says Dr. Hagemeister, is Progression-Free Survival, and since most patients would say they would like to go as long as possible between treatments, Rituxan Maintenance should be considered. He was at the conference to speak in favor of RM, and thinks there is still a role for maintenance for certain patients. (Dr. Hagemeister gets extra points for saying that patients should have a voice in choosing treatments, as long as they have all of the information to make a good decision. And while he doesn't necessarily label it this way, I think he sees the importance of the emotional factor that goes into making this decision. Follicular Lymphoma is an emotional disease as well as a physical one -- I like to hear a doctor who recognizes that.)
Nathan Fowler, MD, and Sagar Lonial, MD, on Treating Follicular Lymphoma
This video has a pretty general title, but there really is more of a focus to it -- Dr. Fowler and Dr. Lonial discuss how to treat Follicular Lymphoma which is refractory or relapsed "early" (which they define as within 2 years after treatment). Dr. Fowler presented at the conference on the recent studies that showed that patients who relapsed within 2 years after receiving R-CHOP had shorter median Overall Survivals. He refers to Dr. Bruce Cheson's talk about PET scans -- a PET at diagnosis can offer a baseline to compare to, if a PET is then taken after treatment. PET scans after treatment can help determine if a patient is likely to be in that POD24 group. Dr. Fowler lists some of the choices that patients have if they are in that "early" group, including Bendamustine, Idilisib, and Obinituzimab. Still, the choice is tough. Dr. Fowler's own personal approach is to try Bendamustine if R-CHOP fails, and if Bendamustine fails within 18 months, he would seriously consider a transplant.
So, some interesting videos, mostly summarizing some of the recent advancements in the field.
Also, I love the ukulele music. I was so distracted by Dr. Cheson's cool shirt in the last video from two weeks ago that I didn't even notice the music.
My dream is to have a job that has conferences in Hawaii. Until that happens, I couldn't think of a group of people (oncologists and cancer researchers) that deserves it more.
Treating FL
https://vimeo.com/174702741
Monday, August 8, 2016
Olympics Inspiration
This post is only a little bit about cancer.
I'm really enjoying the Rio Olympics. For all the fears of things that might happen (and that have happened) outside of the court/track/arena/pool, the athletic competitions have been pretty great so far. And the TV coverage has been kind of uneven, but the network has highlighted some great stories.
*********************
But before I get to that, I have to tell you about my favorite Olympian -- Mary Lou Retton.
Mary Lou won the individual all-around gold medal in gymnastics in 1984. She was the first non-Eastern European to win that gold. She was incredibly popular, not just because she was so great at her sport, but also because she always, always had a smile in her face.
Sometime in the mid-1990's, I got the chance to meet Mary Lou Retton, briefly. I don't remember the year, but I was living in Louisville, Kentucky, at the time, and my oldest child wasn't born yet. So I'll guess 1995 or so.
Mary Lou was on a promotional tour for Tyson Chicken at the time. She made an appearance at our local shopping mall. They had set up a kitchen in the middle of the mall, and my wife and I sat in the audience. (My wife sat very reluctantly. She thought I had a crush on Mary Lou. Ridiculous. I only admired her athletic ability, and her positive spirit. The fact that she was cute as a button had nothing to do with it.) A small screen in the "kitchen" showed highlights of Mary Lou's career, and the film finished with her sticking a landing, her arms raised high. And then -- Mary Lou herself popped out, arms raised high!
She demonstrated a few recipes and talked about healthy eating.
Afterwards, we were given a small cookbook of chicken recipes from Tyson. Here's a picture; you can get it yourself for $2.75:
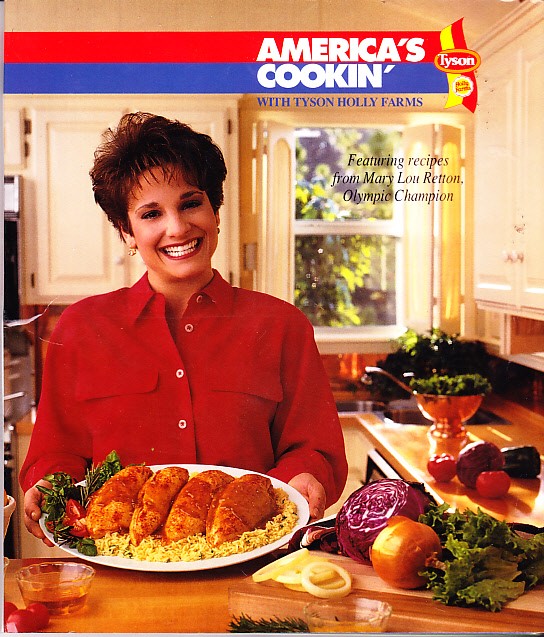
The Orange Chicken recipe is a Must Try!
We were also given the opportunity to get an autograph. Most people were polite and gave Mary lou their name, got their autographed picture, and moved on. That's what my wife did when she went ahead of me. But then she looked back and saw me taking a little extra time to chat with Mary Lou -- probably more than most people did. But I needed to tell her that I appreciated that she was always so happy, when some of those other young athletes just looked miserable. And I was glad she was seemed so happy then, too. She thanked me. My wife thought I was being creepy, but I was sincere. If you've read this blog for a while, you know how much I value someone who is positive.
And I got my autographed picture. It's in a safe place, and I don't want to take it out and copy it, so I'll show you someone else's autographed picture from that same Tyson Chicken promotional tour:

***********************************
I told you that so I can tell you about the most amazing athlete in the Rio Olympics, in my opinion: Oksana Chusovitina, who is a 41 year old gymnast.
41 years old!
Chusovitina was born in Uzbekistan, after the Soviet Union came apart, she competed in the 1992 Olympics for the Unified team, made up of former Soviet countries. Then she competed for Uzbekistan in 1996, 2000, and 2004. The she moved to Germany and competed for them in 2008 and 2012. Now she's back at Rio, competing for Uzbekistan again. (That's 3 different teams.)
And did I mention she is 41 years old!
Know what I was doing at 41? I wasn't competing in Olympic gymnastics, that's for sure. Mostly, I was having cancer and eating ice cream.
She won a team gold medal at the 1992 Olympics, and a silver in the vault in 2008, when she was 33 years old. She's also had 5 moves named after her -- two on the vault, two on uneven bars, and one on floor.
And if you're looking for a blood cancer angle here, it is this: she moved to Germany because her son was diagnosed with leukemia. She paid for the treatment in part by winning gymnastics competitions.
I just can't over the fact that she can do the kind of things she can do at her age, especially when most of her competition is about as old as her 16 year old son. She's pretty inspirational, isn't she? If she can train every day for the Olympics at her age, surely the rest of us can get to the gym for a half hour, three days a week, and make ourselves healthier.
Back to Follicular Lymphoma next time. But for now, I just have to admire this woman a little bit more.
I'm really enjoying the Rio Olympics. For all the fears of things that might happen (and that have happened) outside of the court/track/arena/pool, the athletic competitions have been pretty great so far. And the TV coverage has been kind of uneven, but the network has highlighted some great stories.
*********************
But before I get to that, I have to tell you about my favorite Olympian -- Mary Lou Retton.
Mary Lou won the individual all-around gold medal in gymnastics in 1984. She was the first non-Eastern European to win that gold. She was incredibly popular, not just because she was so great at her sport, but also because she always, always had a smile in her face.
Sometime in the mid-1990's, I got the chance to meet Mary Lou Retton, briefly. I don't remember the year, but I was living in Louisville, Kentucky, at the time, and my oldest child wasn't born yet. So I'll guess 1995 or so.
Mary Lou was on a promotional tour for Tyson Chicken at the time. She made an appearance at our local shopping mall. They had set up a kitchen in the middle of the mall, and my wife and I sat in the audience. (My wife sat very reluctantly. She thought I had a crush on Mary Lou. Ridiculous. I only admired her athletic ability, and her positive spirit. The fact that she was cute as a button had nothing to do with it.) A small screen in the "kitchen" showed highlights of Mary Lou's career, and the film finished with her sticking a landing, her arms raised high. And then -- Mary Lou herself popped out, arms raised high!
She demonstrated a few recipes and talked about healthy eating.
Afterwards, we were given a small cookbook of chicken recipes from Tyson. Here's a picture; you can get it yourself for $2.75:
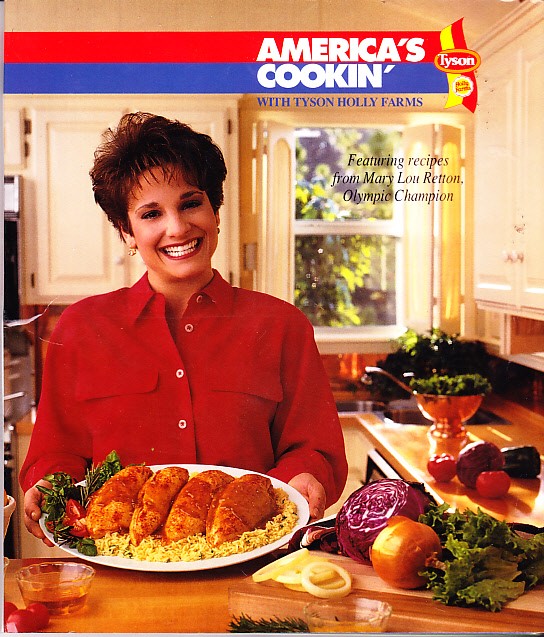
The Orange Chicken recipe is a Must Try!
We were also given the opportunity to get an autograph. Most people were polite and gave Mary lou their name, got their autographed picture, and moved on. That's what my wife did when she went ahead of me. But then she looked back and saw me taking a little extra time to chat with Mary Lou -- probably more than most people did. But I needed to tell her that I appreciated that she was always so happy, when some of those other young athletes just looked miserable. And I was glad she was seemed so happy then, too. She thanked me. My wife thought I was being creepy, but I was sincere. If you've read this blog for a while, you know how much I value someone who is positive.
And I got my autographed picture. It's in a safe place, and I don't want to take it out and copy it, so I'll show you someone else's autographed picture from that same Tyson Chicken promotional tour:

***********************************
I told you that so I can tell you about the most amazing athlete in the Rio Olympics, in my opinion: Oksana Chusovitina, who is a 41 year old gymnast.
41 years old!
Chusovitina was born in Uzbekistan, after the Soviet Union came apart, she competed in the 1992 Olympics for the Unified team, made up of former Soviet countries. Then she competed for Uzbekistan in 1996, 2000, and 2004. The she moved to Germany and competed for them in 2008 and 2012. Now she's back at Rio, competing for Uzbekistan again. (That's 3 different teams.)
And did I mention she is 41 years old!
Know what I was doing at 41? I wasn't competing in Olympic gymnastics, that's for sure. Mostly, I was having cancer and eating ice cream.
She won a team gold medal at the 1992 Olympics, and a silver in the vault in 2008, when she was 33 years old. She's also had 5 moves named after her -- two on the vault, two on uneven bars, and one on floor.
And if you're looking for a blood cancer angle here, it is this: she moved to Germany because her son was diagnosed with leukemia. She paid for the treatment in part by winning gymnastics competitions.
I just can't over the fact that she can do the kind of things she can do at her age, especially when most of her competition is about as old as her 16 year old son. She's pretty inspirational, isn't she? If she can train every day for the Olympics at her age, surely the rest of us can get to the gym for a half hour, three days a week, and make ourselves healthier.
Back to Follicular Lymphoma next time. But for now, I just have to admire this woman a little bit more.
Tuesday, August 2, 2016
Staging Lymphoma with PET Scans
ASCO Post has a great video featuring a discussion between Dr. Julie Vose and Dr. Bruce Cheson. (Of course I'm going to think it's great -- it features Dr. Bruce Cheson!) The discussion took place at the 2016 Pan Pacific Lymphoma Conference in Hawaii (which explains Dr. Cheson's great shirt, though I wouldn't be surprised if he wore a shirt like that all the time, just because it made him happy).
The video looks at how lymphoma is staged -- that is, how oncologists determine how widespread the disease is in the body. They look especially at how PET scans can play a role (or not play a role) in staging.
Scans have become more controversial over the last few years. There seems to be some agreement among oncologists that scans are a good idea for initial staging -- figuring out where the disease is in the body, to help determine the best course of treatment. There is much less agreement on how useful scans are after that point (though most oncologists see some value in a scan after treatment, as a way of measuring how well things went since that initial scan at diagnosis).
This doesn't even get into the problems with scans to begin with -- there's a lot of room for different people to administer and read scans in different ways, making them tough to compare.
(Lymphomation.com has some basic information about PET scans that is worth looking at if you need some background.)
In the video, Dr. Cheson and Dr. Vose discuss some of the history of PET scans, as well as some of the other tests used before (including one that involved injecting blue dye between a patient's toes -- makes drinking those barium milkshakes seem like fun). It wasn't until about 2007 that PET scans became an expected part of staging (which is interesting to me, since I was diagnosed, and scanned, shortly after that).
Dr. Cheson mentions that CT scans with contrast don't do much better than CT scans without contrast, though the contrast ends up giving 50% more radiation to the patient, and is more expensive. there are some situations where contrast helps, but mostly it doesn't.
In addition, PET scans can replace Bone Marrow Biopsies in some lymphomas. (Unfortunately, Follicular Lymphoma isn't one of them -- we still need that BMB.)
Scans are most useful about 6-8 weeks after treatment, since it can take that long for inflammation to come down. This post-treatment scan is known as a "re-staging scan."
However, routine scans after that re-staging scan are discouraged. They rarely pick up that the disease has progressed. In fact, about 80% of the time, a patient is the first one to pick up a symptom and report it to the oncologist. Having a scan once a year is unlikely to find something before a patient notices some kind of change. Routine scans only add radiation to -- and subtract money from -- the patient.
All in all, a pretty interesting video, with some good reminders about when scans are useful, and why we shouldn't rely on them too much.
Plus -- that shirt!
The video looks at how lymphoma is staged -- that is, how oncologists determine how widespread the disease is in the body. They look especially at how PET scans can play a role (or not play a role) in staging.
Scans have become more controversial over the last few years. There seems to be some agreement among oncologists that scans are a good idea for initial staging -- figuring out where the disease is in the body, to help determine the best course of treatment. There is much less agreement on how useful scans are after that point (though most oncologists see some value in a scan after treatment, as a way of measuring how well things went since that initial scan at diagnosis).
This doesn't even get into the problems with scans to begin with -- there's a lot of room for different people to administer and read scans in different ways, making them tough to compare.
(Lymphomation.com has some basic information about PET scans that is worth looking at if you need some background.)
In the video, Dr. Cheson and Dr. Vose discuss some of the history of PET scans, as well as some of the other tests used before (including one that involved injecting blue dye between a patient's toes -- makes drinking those barium milkshakes seem like fun). It wasn't until about 2007 that PET scans became an expected part of staging (which is interesting to me, since I was diagnosed, and scanned, shortly after that).
Dr. Cheson mentions that CT scans with contrast don't do much better than CT scans without contrast, though the contrast ends up giving 50% more radiation to the patient, and is more expensive. there are some situations where contrast helps, but mostly it doesn't.
In addition, PET scans can replace Bone Marrow Biopsies in some lymphomas. (Unfortunately, Follicular Lymphoma isn't one of them -- we still need that BMB.)
Scans are most useful about 6-8 weeks after treatment, since it can take that long for inflammation to come down. This post-treatment scan is known as a "re-staging scan."
However, routine scans after that re-staging scan are discouraged. They rarely pick up that the disease has progressed. In fact, about 80% of the time, a patient is the first one to pick up a symptom and report it to the oncologist. Having a scan once a year is unlikely to find something before a patient notices some kind of change. Routine scans only add radiation to -- and subtract money from -- the patient.
All in all, a pretty interesting video, with some good reminders about when scans are useful, and why we shouldn't rely on them too much.
Plus -- that shirt!